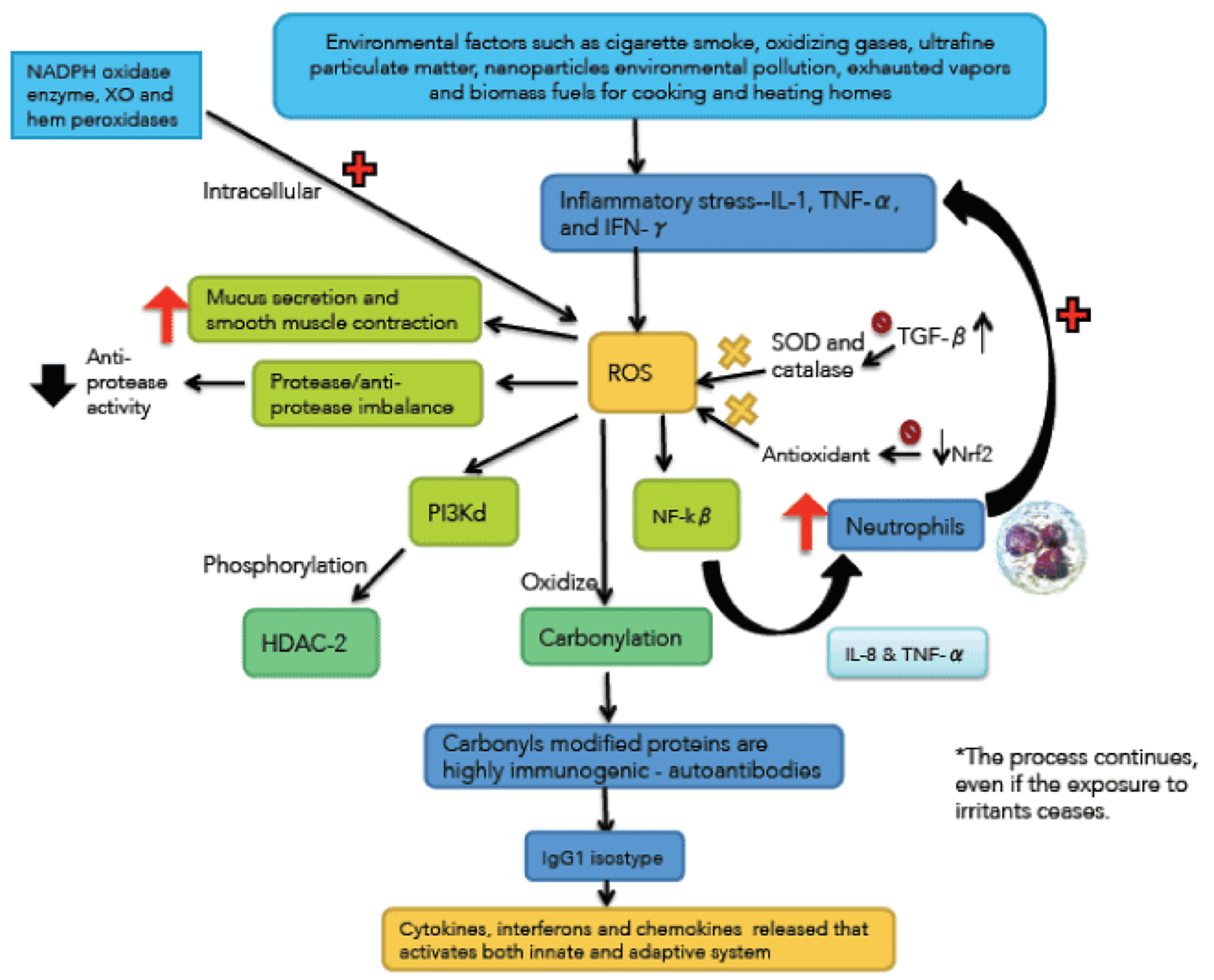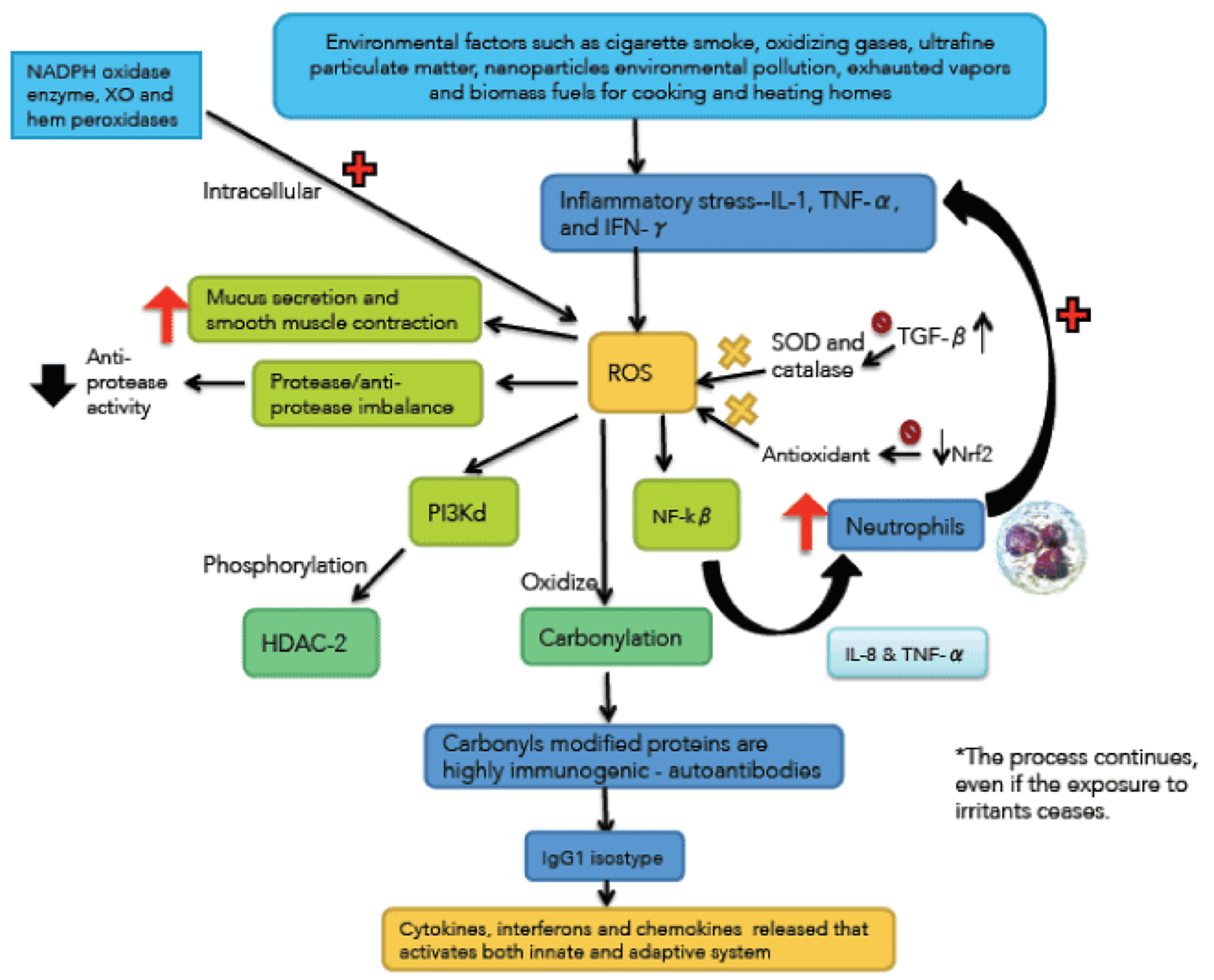
Figure 1. Immunological and inflammatory profile in COPD. Environmental factors produce different types of stress that generates small airways lesion and emphysema, activation of inflammatory cells and autoimmunity. Neutrophils generate more inflammatory stress and autoimmunity actives immune responses that amplify and perpetuate the inflammatory process. The negative sign means repression and positive sign activation. Straight arrows mean increase. Curves arrows mean activation and/or expression.
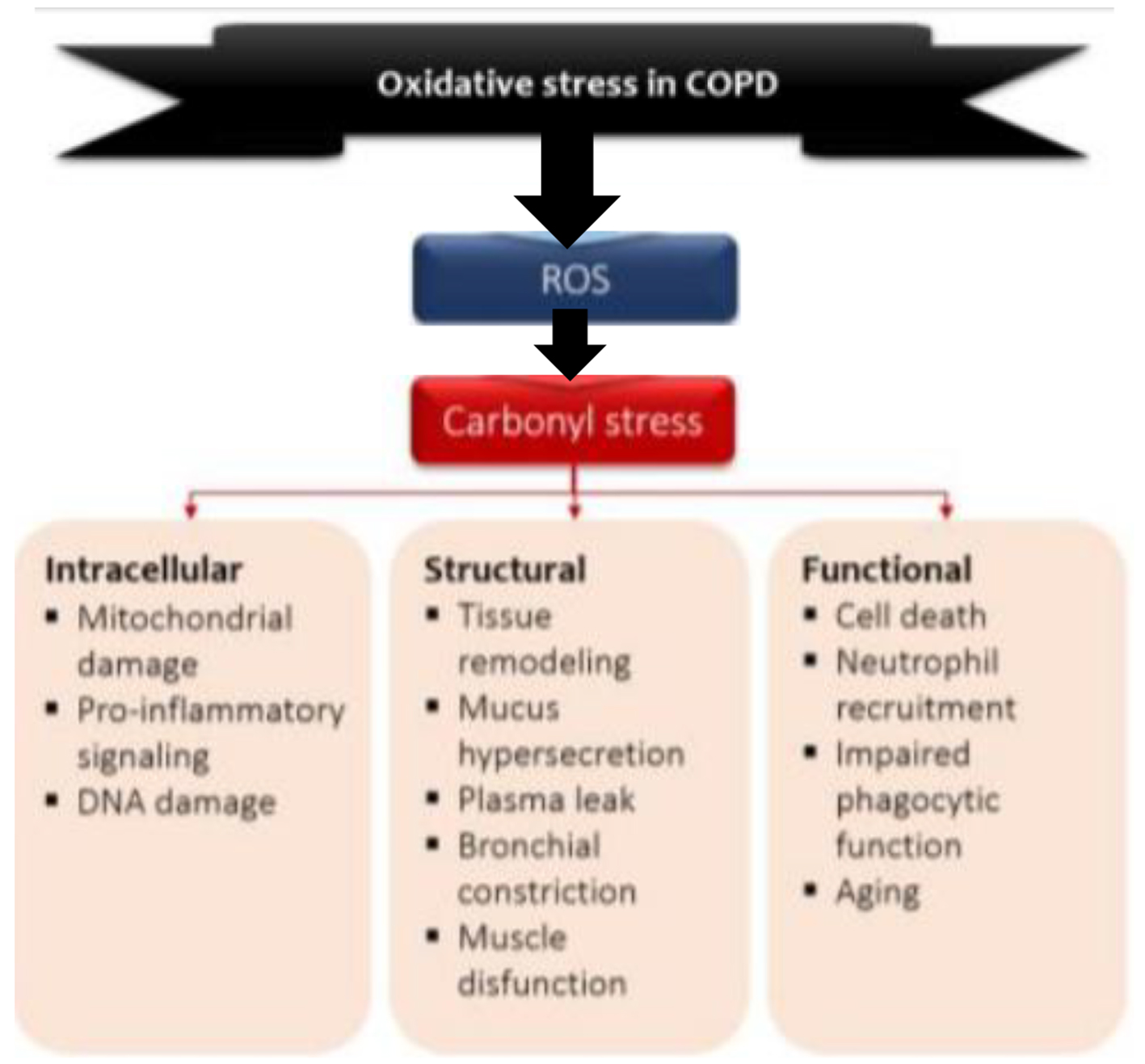
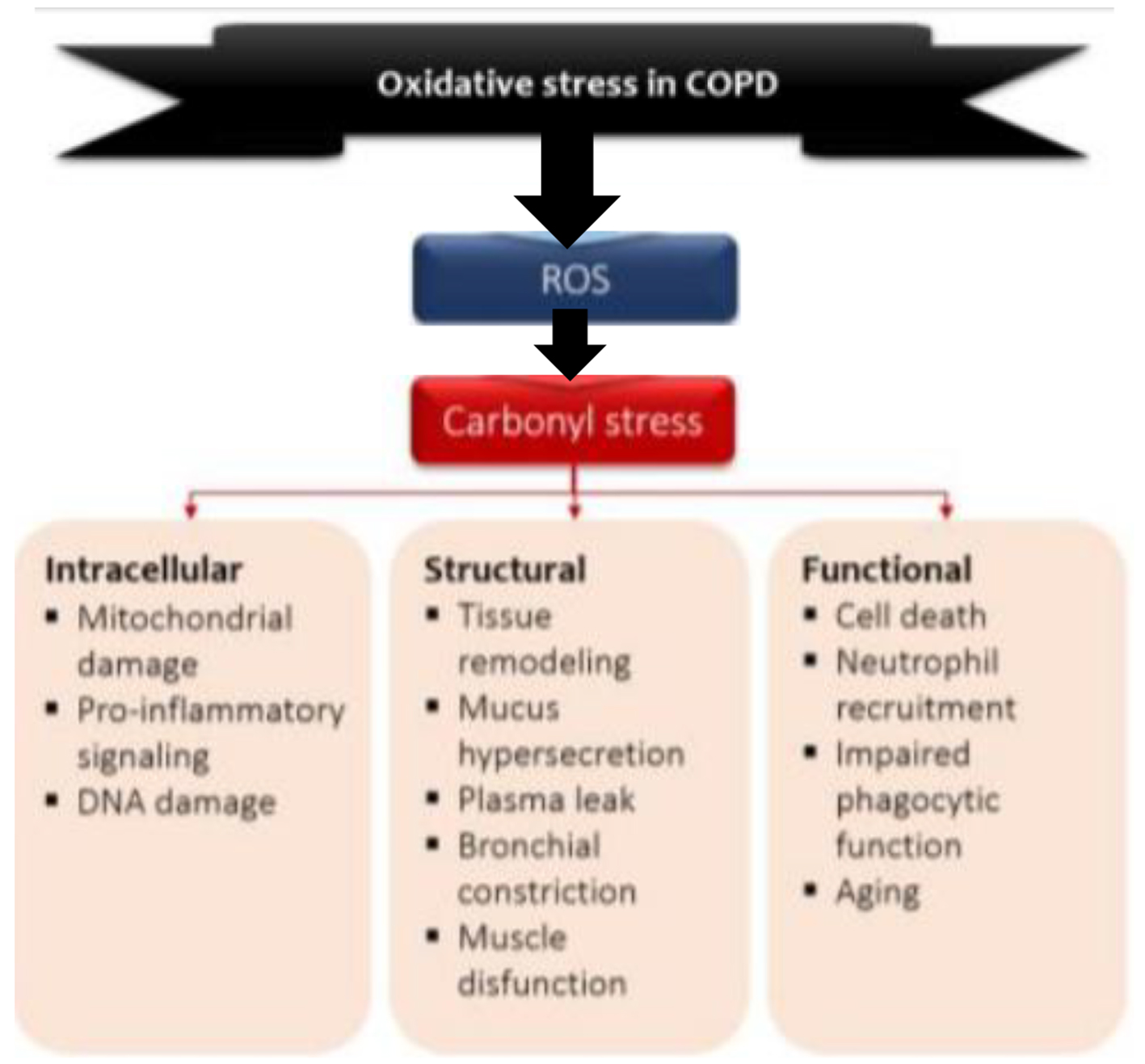
Figure 2. Model of the role of oxidative stress in COPD. Environmental and endogenous sources of reactive oxygen species (ROS) cause lipid peroxidation and the oxidation of proteins and carbohydrates, leading to carbonyl stress. Carbonyl stress in turn produces detrimental intracellular, structural and functional process. O2•: superoxide radical; OH•: hydroxyl radical; ONOO•: peroxylnitite; H2O2: hydrogen peroxide.
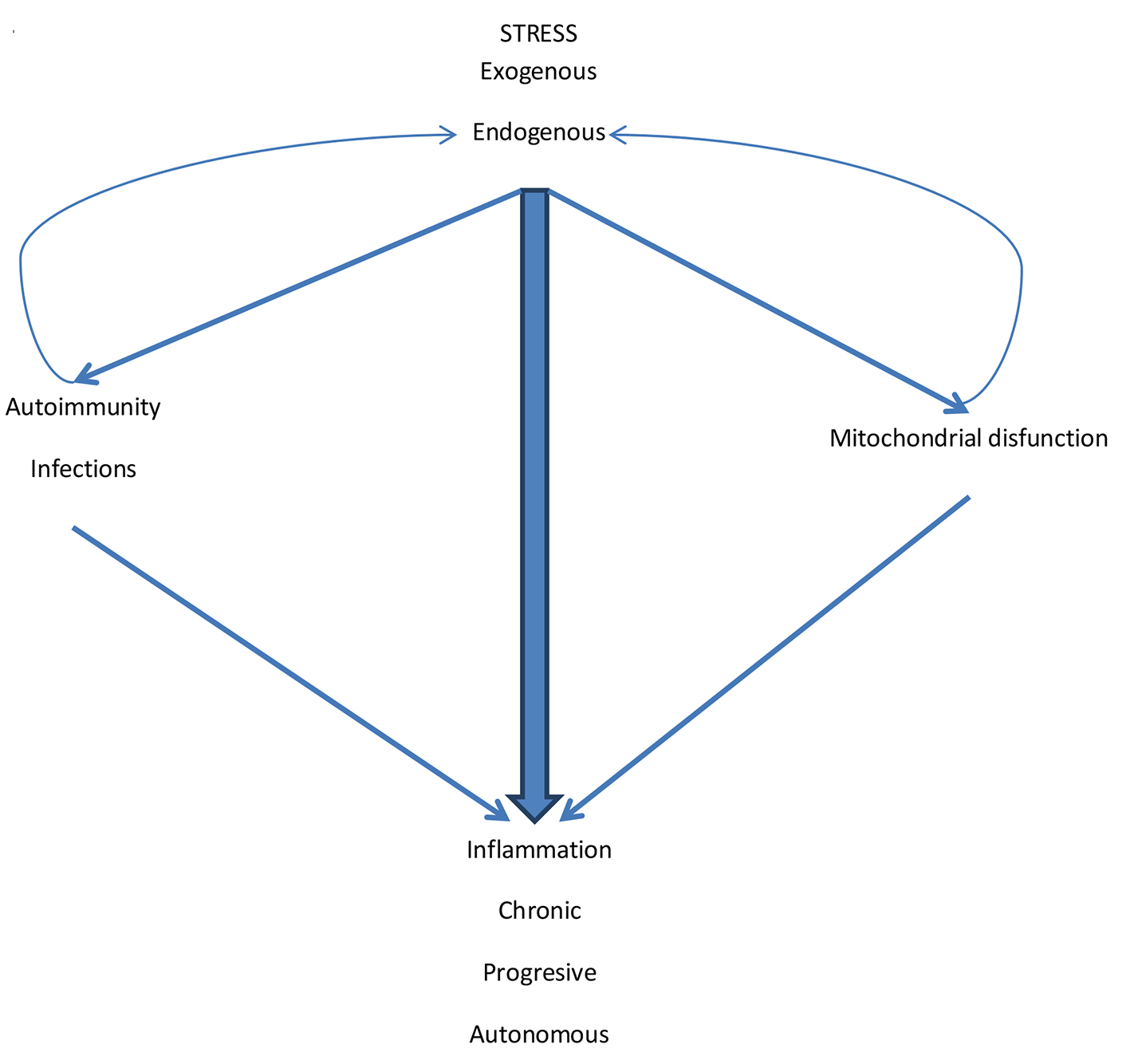
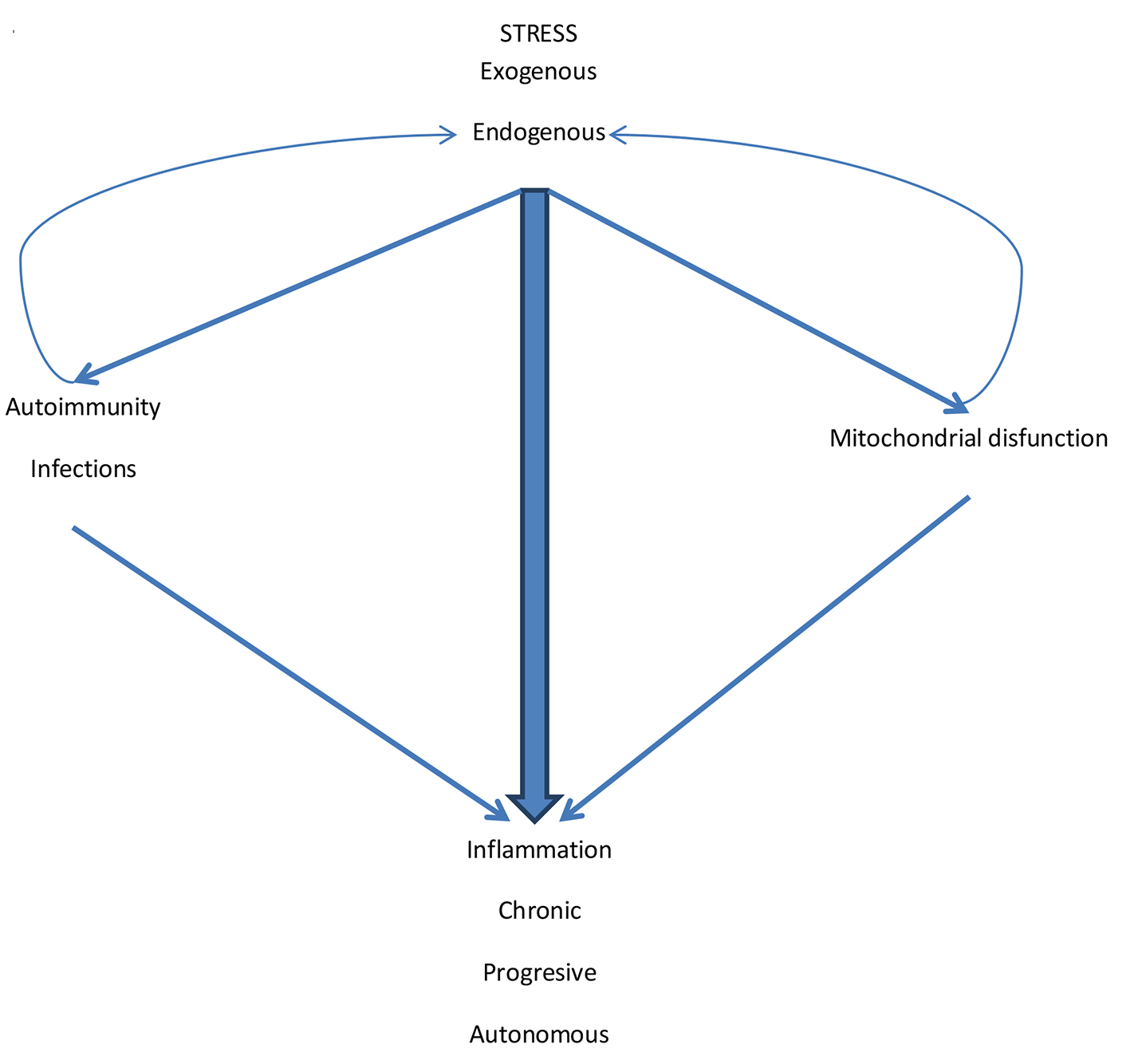
Figure 3. The pathogenic mechanisms of inflammation in COPD. Exogenous stress initiates the inflammatory process. Endogenous stress perpetuates it. Although the external stimulus (CS and other pollutants/biomass fuels) is suspended, endogenous stress and cyclic infections facilitate autoimmunity. Also the various types of stress generate mitochondrial dysfunction. Autoimmunity and mitochondrial dysfunction generate more inflammation but also increase endogenous stress by amplifying the inflammatory process that becomes chronic, progressive and autonomous.